Take it offline!
This Education in Motion resource is also available as a printable PDF.
Download PDF
Updated December 2023
Combining the evaluation and assessment process with the coding, coverage, and payment policies and regulations.
Per Medicare guidelines, the provision of Mobility Assistive Equipment (MAE) is complex and involves multiple components that must be completed in order to qualify a patient for coverage and reimbursement. The National Coverage Determination (NCD) for Mobility Assistive Equipment (MAE) provides the decision algorithm for funding decisions. The algorithm includes the spectrum of technology from walking aids to power wheelchairs and it is necessary to rule out lower levels of technology in order to qualify for the recommended base device.
This guide is intended to assist healthcare providers by providing an overview of those components - coverage, coding, and documentation - as it relates to adult complex rehab power wheelchairs. It is NOT a substitute for the policy itself and should only be relied upon as a quick reference guide. Healthcare providers should familiarize themselves with the Local Coverage Determination (LCD) and related Policy Article for each of the items being recommended in order to obtain a thorough understanding of the Medicare rules and regulations governing mobility assistive equipment.
Basic Funding Elements Specific to Complex Rehab Technology (CRT) Power Mobility Devices (PMDs)
The following provides specific requirements for power mobility devices and CRT wheelchairs in particular:
- The PMD Local Coverage Determination (LCD) and policy article.
- A face-to-face evaluation must be completed and a 7-element written order provided to the supplier.
- The PMD LCD requires a specialty evaluation for power wheelchair bases classified as CRT.
- The PMD LCD requires a RESNA certified ATP to be "direct and in-person" and actively involved in the selection of the technology.
- Policy also requires the OT or PT who completes the specialty evaluation to have no financial tie to the supplier of the technology.
PMD Process Timelines
- Completion of the face-to-face or discharge from a hospital or nursing home stay.
- Supplier involvement follows face-to-face or referral to PT/OT for completion of the evaluation.
- 7-element order (7-EO)
- Supplier must receive the written report of the face-to-face exam within 45 days of completion of the exam or discharge if the examination was performed during a hospital or nursing home stay and prior to delivery of the wheelchair to the beneficiary.
- On-site home assessment - on or before the date the wheelchair was ordered.
Power Mobility Documentation Checklist
When submitting documentation for funding approval, be sure to include the following:
- Face-to-face medical evaluation - date stamped
- 7-element order* - date stamped
- Detailed product description - date stamped
- Specialty evaluation
- Supplier ATP appraisal - demonstrates direct involvement in selection of equipment
- Copy of RESNA certificate
- OR
- Screen-print/printout of credential verification from RESNA website
- Delivery document
- On-site home assessment
* 7-EO is required for Power Mobility Devices (WOPD) and a 5-EO is needed for some options and accessories that may be billed at the same time.
Power Base/PMD Performance Characteristics
| CHAIR |
TYPE |
GROUP 1 |
GROUP 2 |
GROUP 3 |
GROUP 4 |
GROUP 5 |
| Length |
PWC |
40 inches |
48 inches |
48 inches |
48 inches |
48 inches |
| POV |
48 inches |
48 inches |
|
|
|
| Width |
PWC |
24 inches |
34 inches |
34 inches |
34 inches |
28 inches |
| POV |
28 inches |
28 inches |
|
|
|
| Obstacle Height |
PWC |
20 mm |
40 mm |
60 mm |
75 mm |
60 mm |
| POV |
20 mm |
50 mm |
|
|
|
| Minimum Top End Speed - Flat |
PWC |
3 MPH |
3 MPH |
4.5 MPH |
6 MPH |
4.5 MPH |
| POV |
3 MPH |
4 MPH |
|
|
|
| Range |
PWC |
5 miles |
7 miles |
12 miles |
16 miles |
12 miles |
| POV |
5 miles |
10 miles |
|
|
|
| Dynamic Stability Incline |
PWC |
6 degrees (1:12) |
6 degrees (1:12) |
7.5 degrees (1:10) |
9 degrees (1:8) |
7.5 degrees (1:10) |
| POV |
6 degrees (1:12) |
7.5 degrees (1:10) |
|
|
|
| Fatigue Test on a Level with Slats |
PWC |
200,000 cycles
with 0.5-inch
slats under all
wheels |
200,000 cycles
with 0.5-inch
slats under all
wheels |
200,000 cycles
with 0.5-inch
slats under all
wheels |
200,000 cycles
with 0.5-inch
slats under all
wheels |
200,000 cycles
with 0.5-inch
slats under all
wheels |
| POV |
| Drop Cycles |
PWC |
6,666 drop cycles |
6,666 drop cycles |
6,666 drop cycles |
6,666 drop cycles |
6,666 drop cycles |
| POV |
The listed requirements are the minimums; the actual differences between the minimum requirement and what specific models offer can be significant. In addition, other important performance characteristics, features, and functions are not referenced at all. Understanding how these impact performance for each individual is important.
Selecting the Base - Beyond the Diagnosis
The Medicare policy for Group 3 power wheelchairs is diagnosis driven, but not ICD-10 driven. In addition, it isn't as simple as having a qualifying diagnosis. You will need to understand all routinely encountered environments (home and community) to help determine the drive-wheel configuration:
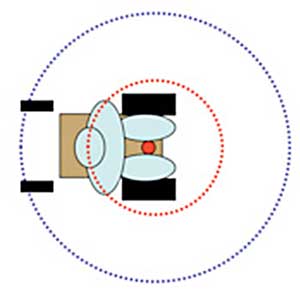
Front-Wheel
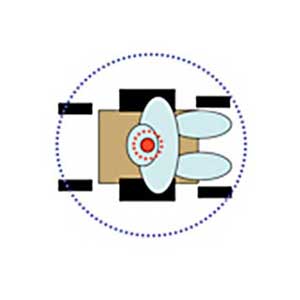
Mid-Wheel
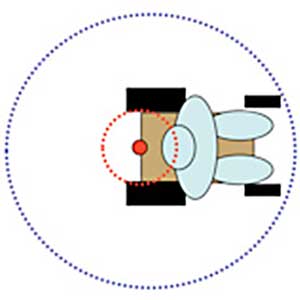
Rear-Wheel
Center of rotation of the chair
Arc described by the head as the chair rotates
Turning radius of the chair
Understanding routine activities, roles, and responsibilities will help define necessary wheelchair performance and influence selection. Don't automatically rule out Group 4 devices; many people may be eligible for Medicaid where community access is a mandate. Also understanding needs and trade-offs will influence final selection, e.g., outdoor performance versus indoor maneuverability.
Characteristics Influencing Base Selection
There are several characteristics that influence base selection. When choosing a base, keep the following in mind:
- Sling or solid base (also known as the rehab seat) - requires additional seat or back cushion. The client must also have a documented medical need for the seating, including the selected seat and/or back cushion. This wheelchair seating policy is ICD-10 driven. Even if the person qualifies for the power wheelchair base, if they do not have one of the listed qualifying ICD-10 diagnoses, the seat or back will be denied.
- Captain seat style - no additional seat or back cushion will be covered.
- Power seating: tilt, recline, elevate, standing
Wheelchair Options, Accessories, and Seating
Important features required to ensure the power wheelchair can meet the person's medical and functional needs will require understanding the wheelchair options and accessories, and wheelchair seating LCDs and associated Policy Articles.
Included in the Initial Payment Group 3 and 4 PWCs
E0978
positioning/safety belt
E0982
tube for pneumatic drive wheel tire
E1225
manual semi-reclining back
E2366
battery charger single-mode
E2367
battery charger dual-mode
E2369
drive wheel gearbox
E2370
integrated drive wheel motor and gearbox combination
E2374
remote joystick replacement
E2375
non-expandable controller
E2376
expandable controller
E2381
pneumatic drive wheel tire
E2382
tube for pneumatic drive wheel tire
E2383
tube for pneumatic drive wheel
E2384
pneumatic caster tire
E2385
tube for pneumatic caster tire
E2386
foam filled drive wheel tire
E2388
foam drive wheel tire
E2390
solid rubber drive wheel tire
E2392
solid caster tire with integrated wheel
E2394
drive wheel excludes tire
E2395
caster wheel excludes tire
E2396
caster fork any size
K0015
non-adjustable height armrest
K0017
adjustable height armrest base
K0018
adjustable height arm - upper portion
K0020
fixed adjustable height armrest pair
K0037
high mount flip up footrest
K0041
large size footplate
K0042
standard size footplate
K0043
footrest, lower extension tube
K0044
footrest, upper hanger bracket
K0045
footrest complete assembly
K0046
elevating leg rest lower extension tube
K0047
elevating leg rest, upper hanger bracket
K0051
can release assembly footrest or leg rest
K0052
swing-away, detachable footrest
K0077
front caster assembly
Coverage and Conditions for Coverage
In order to qualify for power mobility the following conditions must be met:
- Mobility limitation that impairs ability to participate in at least one mobility related activity of daily living. For more details refer to the MAE algorithm.
- The mobility limitation cannot be resolved by the use of a cane, crutches, or walker.
- A manual wheelchair is not an option due to limitations of strength, endurance, range of motion, coordination, presence of pain, deformity, or the absence of both upper extremities and is relevant to the upper extremity function. Even an optimally-configured manual wheelchair is not sufficient to allow the person to perform mobility-related activities of daily living during their typical day.
- Lower level equipment should be trialed or ruled out and documentation should provide specific reasons why they don't meet the person's needs.
Additional coverage criteria for Group 3 PWCs:
- The mobility limitation is due to:
- A neurological condition
- Myopathy
- Congenital skeletal deformity
- Requires a drive control interface other than a hand or chin operated standard joystick.
- OR
- Meets coverage criteria for power tilt or power recline (single-power option) or both (multi-power option) and the system(s) is being used on the wheelchair.
- The person must be willing and have the mental and physical ability to safely use the device or has a caregiver who cannot push an optimally configured manual wheelchair, but is available and able to safely operate the power wheelchair that is provided.
Current seat elevation system coverage (2023)
The individual must undergo a specialty evaluation that confirms the individual's ability to safely operate the seat elevation equipment in the home. This evaluation must be performed by a licensed/certified medical professional such as a physical therapist (PT), occupational therapist (OT), or other practitioner who has specific training and experience in rehabilitation wheelchair evaluations. Also, at least one of the following must apply:
- The individual performs weight-bearing transfers to/from the power wheelchair while in the home, using either their upper extremities during a non-level (uneven) sitting transfer and/or their lower extremities during a sit-to-stand transfer. Transfers may be accomplished with or without caregiver assistance and/or the use of assistive equipment (e.g., sliding board, cane, crutch, walker, etc.).
- The individual requires a non-weight-bearing transfer (e.g., a dependent transfer) to/from the power wheelchair while in the home. Transfers may be accomplished with or without a floor lift or mounted lift.
- The individual performs reaching from the power wheelchair to complete one or more mobility-related activities of daily living (MRADLs) such as toileting, feeding, dressing, grooming, and bathing in customary locations within the home. MRADLs may be accomplished with or without caregiver assistance and/or the use of assistive equipment.
Evaluation and Documentation
The Medicare coverage policy may not include use outside the home, however other funding sources may. For example, Medicaid has a community access mandate.
Document the numerous technology decisions made during the evaluation and technology assessment. Documenting what influenced the decision and how each recommended item impacts the function of the individual is critical for:
- Assisting the individual in understanding the trade-offs related to the final technology decision and in determining whether alternative sources of funding should be sought
- Medical review - without clear and full details, medical review staff may not approve all of the necessary technology
- Appeals
- Legal challenges
Documenting Medical Need
It is necessary to paint a full and detailed picture of the individual's specific needs. Therefore, it is important to include the following types of information in the documentation:
- Physical evaluation and findings, specifically as they relate to the technology recommendation
- Description of any trials or simulations; failings and successes
- Functional needs
- Daily tasks, roles, and responsibilities
- Environments routinely encountered
- Current technology details:
- What worked and what didn't
- Why is replacement necessary; provide details
Start and End with Why
The best way to assess the clarity and sufficiency of the documentation is to ask "why?" Continue to ask "why?" until the answer and details are clear and concise.
Ensure that the final documentation clearly states why the technology choices are necessary, is written objectively, and allows the medical review staff to have a complete and clear picture of the person's needs and how the specific technology recommendations address them.

Replace Subjective and Canned Language with Objective Measures and Details
The importance of the language used in documentation cannot be overstated. Subjective language is open to interpretation and value judgment. There is no guarantee that the medical reviewer, who has not seen the person, will have the same value judgment. Objective language consists of information that is measured and quantified.
Examples of Subjective vs. Objective
Subjective
"The patient is not a functional ambulator."
Objective
- "The patient is unable to ambulate and requires maximal assistance to transfer."
- "The patient is able to ambulate 15' maximum with a walker, which is insufficient for safely moving from the bedroom to the kitchen or to the bathroom in a timely manner."
- "Severe ataxia causes a balance dysfunction for Mr. Jones such that he requires maximal assistance and his wife reports he has fallen twice this month."
Comparing Medical Justification
Example 1
Subjective
"Angle adjustable footrests are required to support lower extremities in a functional position."
Objective
"Mrs. Smith has ankle contractures (supported by measurement of degrees in the evaluation) requiring angle adjustable footplates."
Example 2
Subjective
"A WHITMYER® headrest is needed to maintain neutral alignment and provide support for the head."
Objective
"A WHITMYER Heads Up® with LINX2 hardware is required to inhibit Mr. Jones's asymmetrical tonic neck reflex posturing and to maintain head alignment needed for driving his power wheelchair and other routine activities due to high-tone and spasticity (noted in evaluation)."
Roles in Documentation
Person/caregiver
- Describe daily or routine activities as clearly and as detailed as possible and how the technology will resolve or ameliorate difficulties in performing them.
- Clearly describe current equipment and detail what does or does not meet daily needs.
- Provide details about the various environments/surfaces encountered routinely.
- Provide details regarding transportation, public and private.
Therapist/treating physician
- Document medical and functional limitations and deficiencies.
- Provide details that describe the specific person. Avoid vague generalities or repeating the language in the coverage policy.
- Through words, paint a vibrant and detail picture of the person and their needs.
- Help the reviewer understand the person's daily activities and routine environments and how the recommended technology addresses their needs.
- Document and justify all options, components, and seating being billed to a third party.
Supplier ATP
- List the manufacturer/model name or number for each recommended component on the claim.
- list the technological reasons for choices where applicable (i.e.):
- "Confirmed that LINX2 hardware provides the multi-plane adjustment needed for the intimate fit of the head support pads to adequately position Mr. Jones' head."
- "A center mount Elevated Leg Rest (ELR) is the only style available on the base Mr. Jones needs."
- "Due to high tone and reduced range of motion in knees and hips, traditional 2-sided ELRs are not usable by Mr. Jones. A center mount ELR positions Mr. Jones's feet inside the front asters and therefore allows the knee bend angle and hip angle he requires (supported by the therapist's evaluation)."
- Record all measurements for the wheelchair, seating, and components in the supplier's assessment documentation.
- Document the home or environmental considerations that are limiting choices in technology and why.
- Create and follow a clear process for reviewing documentation and ensuring all required elements are present before submitting. Minimize submission of unnecessary information; it only complicates the review process. Using the checklist provided by the DME MACs is useful.
Power Mobility Resources
- Dear Physician Letter: Power Wheelchairs and Power Operated Vehicles - Documentation Requirements (PDF)
https://www.cgsmedicare.com/jc/pubs/news/2010/0910/cope12954.pdf
- Local Coverage Determination and Policy Article
https://www.cgsmedicare.com/jc/coverage/lcdinfo.html
- Medicare Claim Review Programs: MR, NCCI Edits, MUEs, CERT and Recovery Audit Program (PDF)
http://garnerhealth.com/wp-content/uploads/2014/02/MCRP_Booklet.pdf
- Medical Review Power Mobility FAQs
https://www.cgsmedicare.com/jc/help/faqs/current/cope14455.html
- Mobility Assistive Equipment (MAE)
https://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=219&ncdver=2&bc=AgAAgAAAAAAA&
- National Coverage Determination (NCD)
https://www.cms.gov/medicare-coverage-database/indexes/ncd-alphabetical-index.aspx?bc=BAAAAAAAAAAA
- Power Mobility Devices - 7 Element Order
https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/PMD_DocCvg_FactSheet_ICN905063-text-only.pdf
- Seat Elevation Systems as an Accessory to Power Wheelchairs (Group 3)
https://www.cms.gov/medicare-coverage-database/view/ncacal-decision-memo.aspx?proposed=N&ncaid=309
Documentation Checklists
- Power Mobility: Group 3 No Power Option PWCs (K0848 - K0855), Group 3 Single Power Option PWCs (K0856 - K0860), & Group 3 Multiple Power Option PWCs (K0861 - K0864)
https://www.cgsmedicare.com/pdf/dme_checklists/pmd_3_2018re.pdf
- Power Mobility: Group 5 (Pediatric) PWCs with Single (K0890) or Multiple (K0891) Power Options & Push-Rim Activated Power Assist Device (E0986) for a Manual Wheelchair (PDF)
https://www.cgsmedicare.com/pdf/dme_checklists/pmd_5_2018re.pdf